How EVV Differs State by State
Electronic Visit Verification (EVV) is a digital system that captures accurate and standardized home care appointment information. As an accountability tool designed to reduce fraud within the industry, its primary function is to verify that visits are happening in the right place at the right time.
EVV is mandated at the federal level for all home care agencies that offer specific services billed through Medicaid. However, each state also has its own unique requirements surrounding the implementation of EVV, so things can get complicated fast for agencies that operate across multiple markets.
In this piece, we’ll explore the high-level purpose of EVV and cover more granular state-by-state requirements so you can stay current, compliant, and confident in your operations.
Federal EVV Mandate Overview
The 21st Century Cures Act is the official document that codifies the use of EVV across the United States. In simple terms, it’s used to verify the delivery of Personal Care Services (PCS) and Home Health Care Services (HHCS) according to a set of unified standards.
For PCS, these rules have been in place since January 1, 2020, while HHCS was codified exactly three years later. As of those dates, agencies that don’t comply with federal requirements may be subject to reduced Medicaid funding at the state level; instead of being fined directly, organizations will simply receive fewer subsidies in the future.
State-by-State EVV Requirements
How are these federally legislated rules enforced? The answer varies from state to state. Since they are the ones who control how agencies get paid, they have their own set of rules that govern how EVV must be applied.
One of the most influential EVV considerations is whether an agency is operating in an open model or closed model state. In open model states, they have the flexibility to choose their own EVV vendor as long as it sends data to the state’s designated aggregator. Agencies still need to format their data according to the mandated specifications, and in some cases, smaller organizations can access a free, state-provided option for their EVV needs.
Closed model states, on the other hand, work with a single EVV provider that all agencies must adopt. While this model affords far less freedom on a case-by-case basis, it tends to yield more consistent data and simpler compliance tracking for state governments.
While less common, a hybrid model does exist. In these situations, states mandate one primary vendor for all EVV processing while allowing third-party systems to connect as long as they complete the certification process.
On a more granular level, some states require EVV for more than just PCS and HHCS, including services like respite care, companion care, and homemaking assistance. Some states restrict the number of edits that can be made to a visit log or require extensive documentation when correcting late or incomplete information. The list goes on, and in all cases, these regulations vary significantly from one jurisdiction to another.
Sample State Requirements
California EVV follows an open state model. While the CA government does provide a standardized vendor option, agencies are free to choose their own EVV software. The following service types currently require EVV in California, though exact services may depend on the specific program and policies within the Medi-Cal system:
- Personal care services (PCS)
- In-home supportive services (IHSS)
- Home health care
- Private duty nursing
- Home and community-based services (HCBS)
- Behavioral health services
- Respite care
- Palliative care
- Hospice care
There are certain exceptions wherein California home care agencies may be eligible for an exception or waiver from using the provided EVV state aggregator. These include live-in caregivers, self-directed personal care services (PCS), home health care (HHC), travel time, emergency backup systems, and services provided in rural areas with limited access to internet or cellular service.
Arizona EVV is another open state that follows the same broad strokes as California. The following services are currently mandated for EVV use in Arizona; a more comprehensive list can be found on the Arizona Health Care Cost Containment System (AHCCCS) website.
- Personal care services (PCS)
- Home health care
- Habilitation services
- Respite care
- Attendant care services
- Behavioral health services
- Private duty nursing
- Homemaker services
- Durable medical equipment and supplies (DME)
- Home and community-based services (HCBS)
Arizona’s waivers and exceptions can include technology failure, medical necessity, emergency situations, unique circumstances, provider hardship, and client requests.
Louisiana EVV follows a closed model, requiring all providers to use its single, state-mandated vendor. Agencies must submit visit data directly through the state’s designated system, and third-party EVV solutions are not permitted for official submission.
Services that require EVV in Louisiana typically include:
- Personal care services (PCS)
- Home health care
- Long-term personal support services
- Respite care
- Adult day health care
- Community-based services under specific waiver programs
While the state’s closed-model approach limits vendor flexibility, it standardizes data collection, simplifies auditing, and helps ensure consistent visit verification across all providers. Limited exceptions may apply in circumstances involving system outages, caregiver emergencies, or client safety.
Essential Data Elements & Documentation
No matter which state an agency operates in or which EVV model is used, caregivers must capture the same six elements during every visit to stay compliant: the services being delivered, the name of the individual receiving care, the date, the location, the name of the caregiver providing the service, and the appointment’s start and end time.
If any of these core elements are missing or incomplete, states will typically respond by denying the claim, delaying payment, requesting an amendment, or initiating the audit process.
Training & Operational Best Practices
Running an airtight EVV program requires extensive staff training. If employees aren’t entirely up-to-date on what’s needed for these state-level systems, some information may still fall through the cracks, leaving agencies facing various penalties.
At the outset, caregivers should be shown how to perform basic functions, such as clocking in, clocking out, and recording necessary data, as well as how to amend a visit log and address any applicable exceptions. They should also be educated on the primary benefits of EVV and how these systems keep agencies healthy and thriving.
Following these initial training sessions, periodic refreshers are essential for sharing legislative updates, addressing caregiver questions, reviewing new app features, and ensuring everyone is well-equipped to support your risk reduction efforts.
Frequent Pitfalls & How to Avoid Claim Denials
Most EVV compliance violations fall under a few predictable categories. Incorrect or incomplete documentation is one of the most common issues: entering an incorrect service code, omitting one of the six key elements, or contradictions within a caregiver’s notes can all trigger a denial or delay.
It’s okay for caregivers to amend data from past appointments, but only up to a certain point. If the state flags too many edits on a given record, they might delay the repayment process to investigate further. Agencies can avoid this issue by encouraging caregivers to log their clock-ins and clock-outs in real-time (as opposed to entering their visit hours later) and maintaining timely record-keeping.
Another pitfall that ties back to real-time data logging is location mismatching; something as simple as clocking in from a vehicle instead of the client’s home can raise a flag.
Sometimes, technical difficulties prevent submitted forms from reaching the state’s data aggregator. Maybe there was a file formatting issue, or perhaps a submission didn’t meet the provided deadline. In any event, regularly stress-testing integrations and assigning a staff member to monitor aggregator error logs can go a long way towards preventing technical errors.
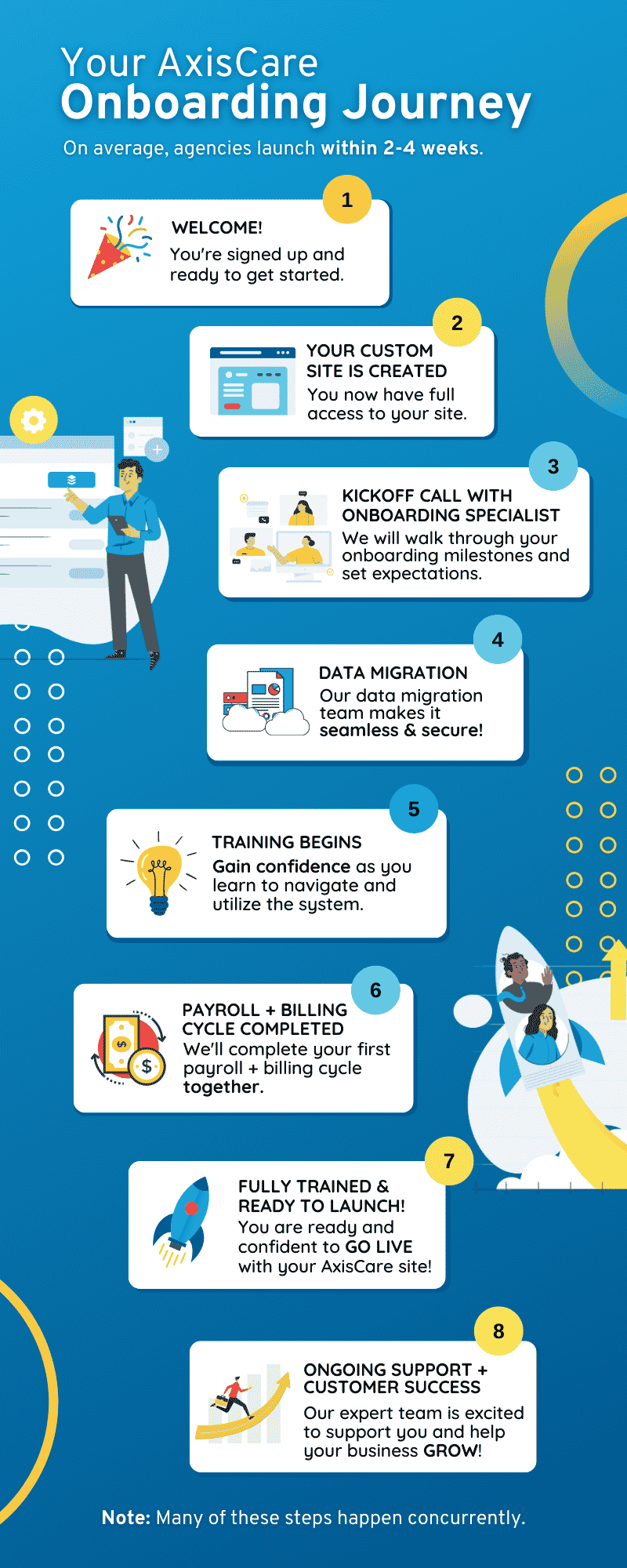
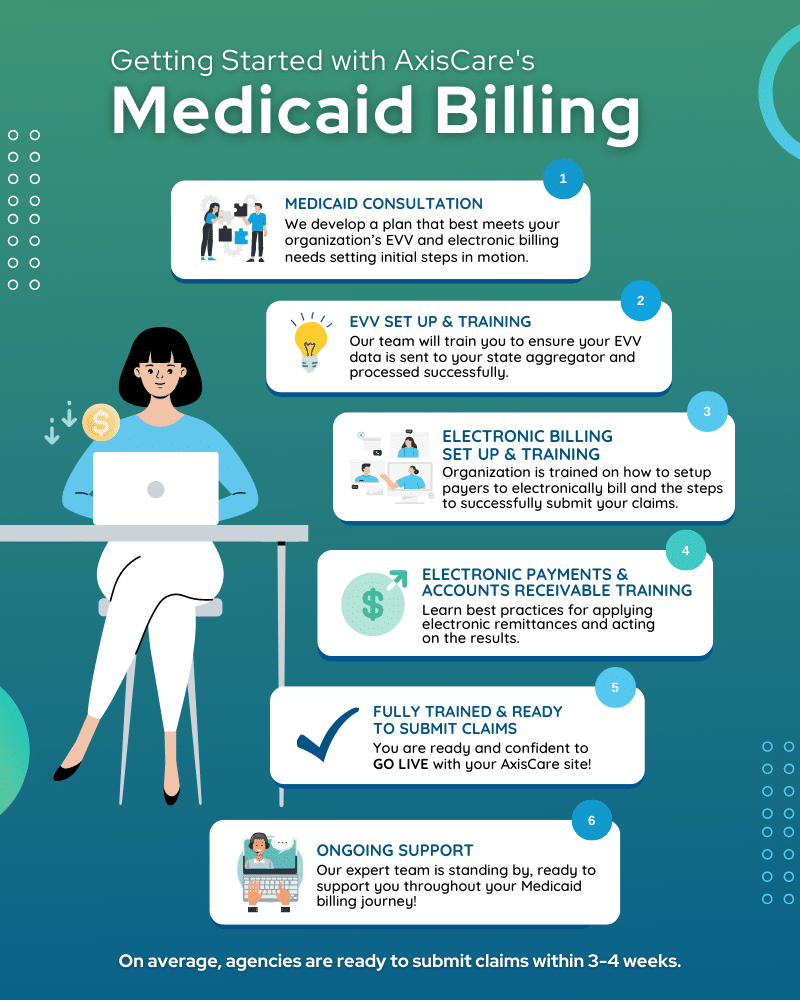
Manage EVV for Each State With AxisCare
AxisCare partners with agencies across the United States to support accurate and compliant EVV, regardless of the model they operate in. Whether your state uses an open, closed, or hybrid system, our platform is designed to integrate seamlessly with state-mandated vendors, aggregators, and data formats.
From standardized documentation to state-specific regulations, we help agencies streamline EVV workflows, reduce errors, and maintain audit readiness. If you’re looking for a system that simplifies compliance in any market, request a live demo with our team and see why agencies nationwide trust AxisCare as their EVV partner.