There’s a rumble being felt throughout our industry, revolutionizing the way we operate, called person-centered care (PCC). This game-changing approach emphasizes the individual, taking their specific needs into account and actively involving them in decision-making processes.
Technically, all healthcare is administered at the individual level. But traditional approaches are less about understanding the patient’s perspective, and more about what the doctor recommends regardless of the circumstances. While PCC is only just starting to shape the care landscape, it has already proven effective at improving patient outcomes, increasing satisfaction, and more.
Key Principles of Person-Centered Care
Sometimes, it can feel like there’s a divide between practitioner and patient. Doctors, being the experts, tend to share information and treatment suggestions that are one-size-fits-most. PCC aims to tear down this wall and enable more personalized solutions by:
Understanding the Patient's Perspective
The patient perspective is the driving force behind PCC, and should serve as the foundation of their care plan. They should be made to feel totally comfortable in their care environment and encouraged to share any information that may inform the practitioner’s recommendations.
Building Trust and Collaboration
Establishing a trust-based relationship will pave the way for effective communication and collaboration; patients should trust that their best interests are being kept in mind, and practitioners should trust patients will adhere to their care plan and be transparent every step of the way.
Tailoring Care Plans to Individual Needs
PCC involves tailoring care on an individualized level, taking into account the patient’s social needs, beliefs, financial situation, and more.
Barriers to Scaling Person-Centered Care
Scaling personalized solutions is a tall order for any industry. Factor in the delicate and often emotional nature of healthcare, and you have yourself a true challenge. Rolling out PCC at scale certainly isn’t impossible, but you’ll need to approach it with eyes wide open.
Limited Resources and Time Constraints
Caregivers and practitioners often find themselves pressed for time, which leaves little room for in-depth conversations and joint decision-making – two crucial elements of PCC.
Overcoming Staff Training Hurdles
Delivering adequate training that properly explains PCC principles and techniques is crucial. Without it, caregivers may feel unsure about how to approach certain conversations or situations, which erodes confidence on both sides.
Strategies for Effectively Scaling Person-Centered Care
When there’s a will, there’s a way. Adopting PCC organization-wide is certainly possible as long as you have a robust strategy in place. Here are a few things to consider as you implement these changes.
Cultivating a Patient-Centric Culture
Transformation begins with a cultural shift that can be encouraged through workshops, strategic hiring initiatives, and enthusiastic buy-in from leadership.
Empowering Healthcare Providers With Training and Resources
Healthcare has been routine for so long that caregivers likely will need guidance when approaching a new care model. Adequate training and resources will get them up to speed on PCC and equip them to deal with delicate topics that come up.
Utilizing Multidisciplinary Teams
Multidisciplinary teams bring together expertise and perspectives from various disciplines. These teams can address complex medical issues from every angle, ensuring a more well-rounded and personalized treatment experience.
The Role of Technology in Expanding Person-Centered Care
Arguably the only successful way to scale your PCC strategy is by leaning on technology, including home care software. The right platform will help you manage your new approach with ease, supported by a suite of features designed to make work simpler for home care agencies.
Telemedicine and Virtual Health Platforms
If PCC is all about the patient, it should be able to accommodate any physical limitations while making care as efficient as possible. Whether an individual is unable to make it to a hospital or in-person visits simply aren’t necessary, telehealth platforms can significantly improve accessibility and convenience for patients.
Wearable Devices and Remote Monitoring
Similarly to telehealth, remote sensors and monitors transmit essential information around the clock. Whenever an aberration is detected, a notification is sent out immediately, enabling faster responses and contributing to a comprehensive patient record.
AI and Machine Learning for Personalized Care Plans
It’s unrealistic to expect overwhelmed caregivers to analyze vast amounts of patient data and extract insights. That’s where AI comes in. Machine learning algorithms can comb huge piles of information in no time, enabling practitioners to quickly and effectively draw up personalized care plans that are tailored to each patient.
Overcoming Resistance to Change
Some internal stakeholders will be excited about the shift towards PCC, while others will certainly have their reservations. Addressing their resistance with calm and understanding attitude and a focus on clarification will go a long way toward winning them over.
Common Concerns and Misconceptions
Acknowledge and provide solutions for common concerns and misconceptions that may impede the acceptance of PCC. Discuss effective strategies to overcome resistance, like clear articulation of the benefits addressing any misconceptions, and highlighting the importance of transparent communication.
Emphasizing the Benefits
Stakeholders shouldn’t have to guess or make assumptions about why PCC is a net positive. Make sure to explain its impact on healthcare providers in detail, including increased job satisfaction and improved patient relationships, and use proof to drive the point home.
Encouraging Open Communication within Organizations
Communication isn’t just a must in a patient-caregiver dynamic. Transparency within healthcare organizations and agencies is just as important for addressing concerns, sharing success stories, and fostering a collaborative approach both during and after implementation.
Future Trends in Person-Centered Care
Clearly, the healthcare space is in constant evolution. New technologies hit the market, attitudes change, and slowly, approaches begin to shift. Here’s what we think it will take for PCC to become the future of home care and beyond.
Continuous Improvement Through Feedback and Data Analysis
The outcomes associated with your PCC program will only get better over time. Soliciting feedback from staff will not only help you optimize your PCC rollout but also improve care delivery as their suggestions are implemented. Put simply, employees that feel heard perform better.
Global Initiatives and Collaborations
According to the World Health Organization, by 2030, one in six people will be aged 60 years or older. All signs are pointing towards home care demand increasing around the world, and for each patient to receive the care they need and deserve, governments and agencies will need to share best practices and tackle the challenge together.
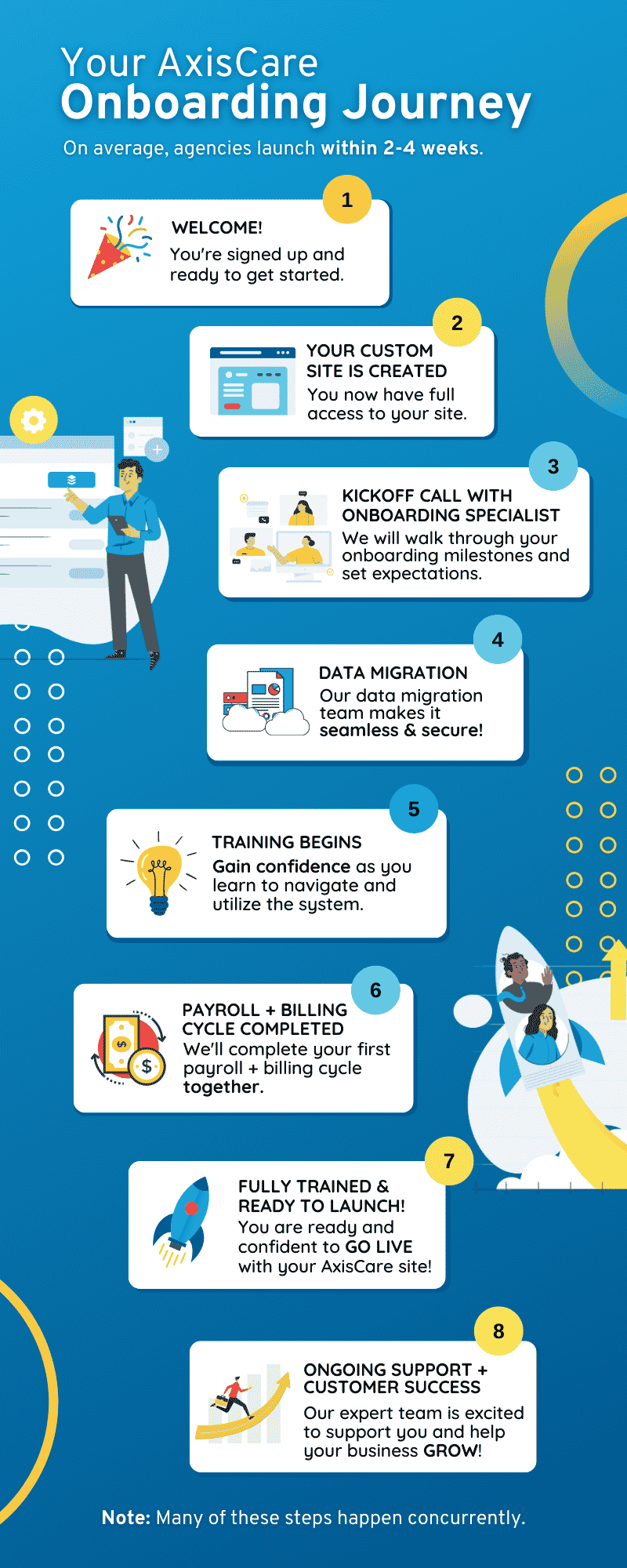
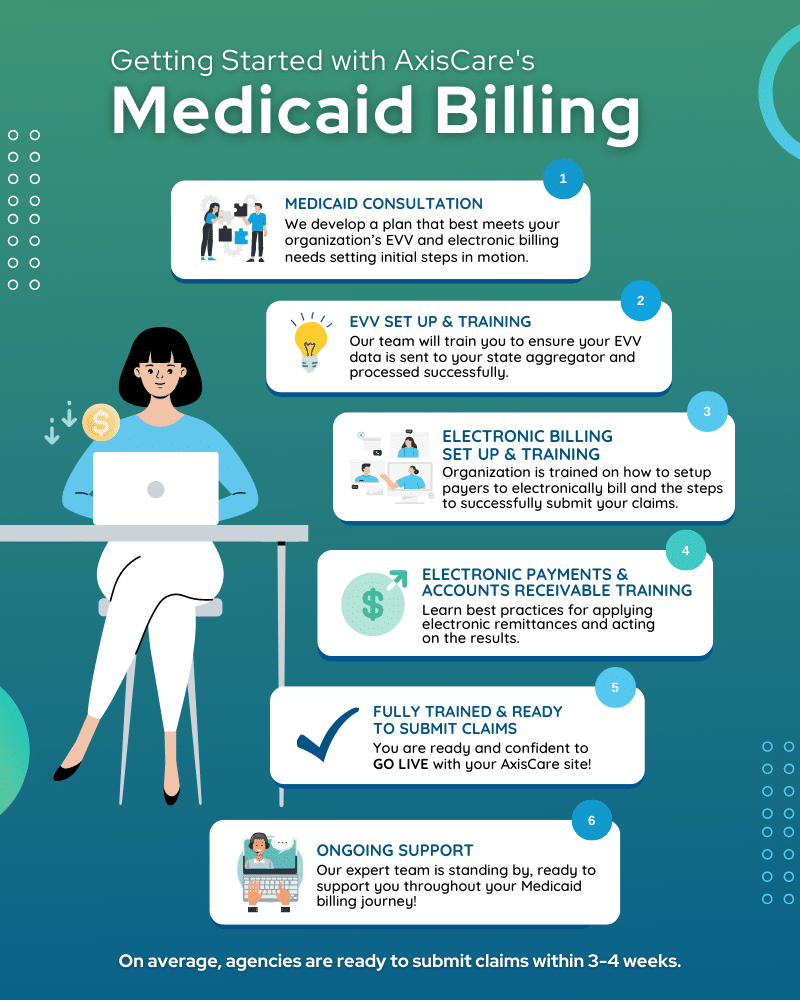
Provide Quality Tailored Care With AxisCare
AxisCare takes work off caregivers’ plates, leaving more time and space to provide ultra-personalized care. Handy features like medication reminders and custom forms automate routine tasks, while client and family portals work to build trust and bolster collaboration. Curious to learn more? Book a live demo!