Person-centered care applies a deeply human approach to the art and science of healthcare. You might be thinking, “Isn’t all care patient-centered because it inherently focuses on the individual’s needs and concerns?” And you wouldn’t be wrong for looking at it that way – but the reality of PCC is much more nuanced.
Understanding Person-Centered Care
Consider the level of autonomy and control we have in our daily lives. As long as we’re healthy and financially stable, we can more or less do as we please and make choices that align with our values.
In a healthcare setting, however, it can sometimes feel like there is a wall between practitioner and patient. Information and treatment recommendations are handed down from doctors – they are the experts, after all – in what feels like a one-size-fits-most solution.
The Importance of PCC in Healthcare
PCC acknowledges individuality on a profound level, creating a more connected relationship between patients and practitioners. It gives patients a greater say in how their care is administered, empowering them as a partner in their care plan and actively seeking their input. To accomplish this goal, PCC considers factors that go beyond a patient’s physical health, such as emotional, social, and financial needs.
Patient-Centered Care vs. Person-Centered Care
All patients are people, but these two types of PCC aren’t exactly alike. Both are focused on breaking down clinical barriers to provide a more collaborative and human framework for care, whether in a traditional or homecare setting, but there are fundamental differences as well.
Patient-Centered Care is largely focused on what happens during doctor’s visits, and often puts a greater emphasis on medical diagnoses, treatment plans, and clinical outcomes. Care is typically structured around the specific medical condition or ailment, with the medical provider remaining in the driver’s seat.
Person-Centered Care, on the other hand, takes into account “the big picture” of one’s lived experience. As we mentioned above, it emphasizes the patient’s overall well-being – not just their physical health. Care is tailored to their unique circumstances, and the patient is invited to actively participate in determining what that plan will look like.
Elements of Person-Centered Care
In short, these are the most important tenets of PCC:
- Respectful and responsive care
- Individualized care plans
- Collaborative and coordinated care
- Accessible care
- Respect for patient and family preferences
The History and Evolution of PCC in Healthcare
For much of modern history, healthcare practitioners have held the ultimate authority and made decisions on behalf of patients without much input. With the advent of Person-Centered Care, we are slowly shifting from a more paternalistic approach to a more patient-centric model. Here’s how the concept has gained ground over time.
1950s
Psychologist Carl Rogers introduced the concept of “client-centered therapy,” an empathetic and non-judgmental technique which ran counter to the norm. At the time, therapists took a more prescriptive approach, which focused on diagnosing patients and leveraging their expertise rather than creating a space where patients could express themselves freely.
1960s-1970s
The civil rights movement and disability rights movements brought diverse and marginalized voices to the forefront, encouraging society to reevaluate current frameworks.
1980s
The World Health Organization (WHO) began promoting patient-centered care as a fundamental principle of healthcare.
1990s
The Institute of Medicine (now the National Academy of Medicine) released several reports highlighting the need for patient-centered care in healthcare reform efforts. These reports were a clear and authoritative call to action for reform, putting forth specific recommendations and guidelines that would help shape the PCC landscape for decades to come.
2000s
Various healthcare organizations, including the Institute for Healthcare Improvement (IHI) and the Picker Institute, began promoting PCC principles.
Technology Advancements
Advances in healthcare technology, such as telemedicine and mobile health apps, have further empowered patients to engage in their care and access to information.
Benefits of Person-Centered Care
There are numerous advantages associated with PCC. Let’s explore what happens when healthcare organizations prioritize individuals’ needs, preferences, and values, placing them at the center of their experience.
Improved Patient Outcomes
PCC can lead to increased adherence to treatment regimens, since patients are more likely to follow a plan that they have actively participated in creating.
Enhanced Patient Satisfaction
Person-centered care encourages open and honest communication between patients and healthcare providers. The more that patients feel heard, seen, and considered, the more confident they’ll feel in the care they’re receiving and its ability to improve their situation.
Lower Healthcare Costs
When care is tailored to a patient’s specific needs and priorities, resources are allocated more efficiently. Unnecessary tests, treatments, and medications that can drive up healthcare costs are minimized.
Increased Quality of Care
Healthcare providers can create personalized care plans that take into account the patient’s unique circumstances, leading to more effective and appropriate treatments.
Challenges and Barriers to PCC
These challenges can hinder the successful adoption and integration of PCC principles into healthcare systems.
Time Constraints
Healthcare providers often have tight schedules, with limited time allocated for each patient. This can make it challenging to engage in in-depth discussions and shared decision-making, which are central to PCC.
Lack of Training and Education
Many healthcare professionals may not have received adequate training in PCC principles and techniques. This can result in a lack of confidence in implementing person-centered approaches, or uncertainty surrounding how to approach certain conversations.
Resistance to Change
Change is rarely easy to implement. Some healthcare providers may resist adopting PCC because it requires a shift from a traditional, paternalistic model of care to one that values patient autonomy and shared decision-making.
Cultural and Language Barriers
In multicultural healthcare settings, such as large cities, language and cultural differences can create barriers to effective communication and understanding between healthcare providers and patients.
Implementing PCC in Healthcare
The good news is, the above challenges can be overcome with a well thought-out and robust strategy. Here are the pillars that healthcare organizations should be considering when looking to implement PCC as a solution.
Cultural Transformation
Healthcare institutions must embrace a culture that prioritizes patient-centeredness. Cultural shifts are often slow and steady; they can be encouraged through training workshops, strategic hiring initiatives, and engaging leadership members to support the changes.
Care Planning
Develop individualized care plans that consider the patient’s unique needs, values, and goals, and involve patients in setting treatment goals
Communication and Collaboration
Healthcare providers should practice active listening, empathy, and clear communication to build trust and rapport with patients.
Patient Feedback
Collect feedback from patients through surveys, focus groups, and other means to assess the patient experience and identify areas for improvement.
Embrace PCC in Healthcare With AxisCare
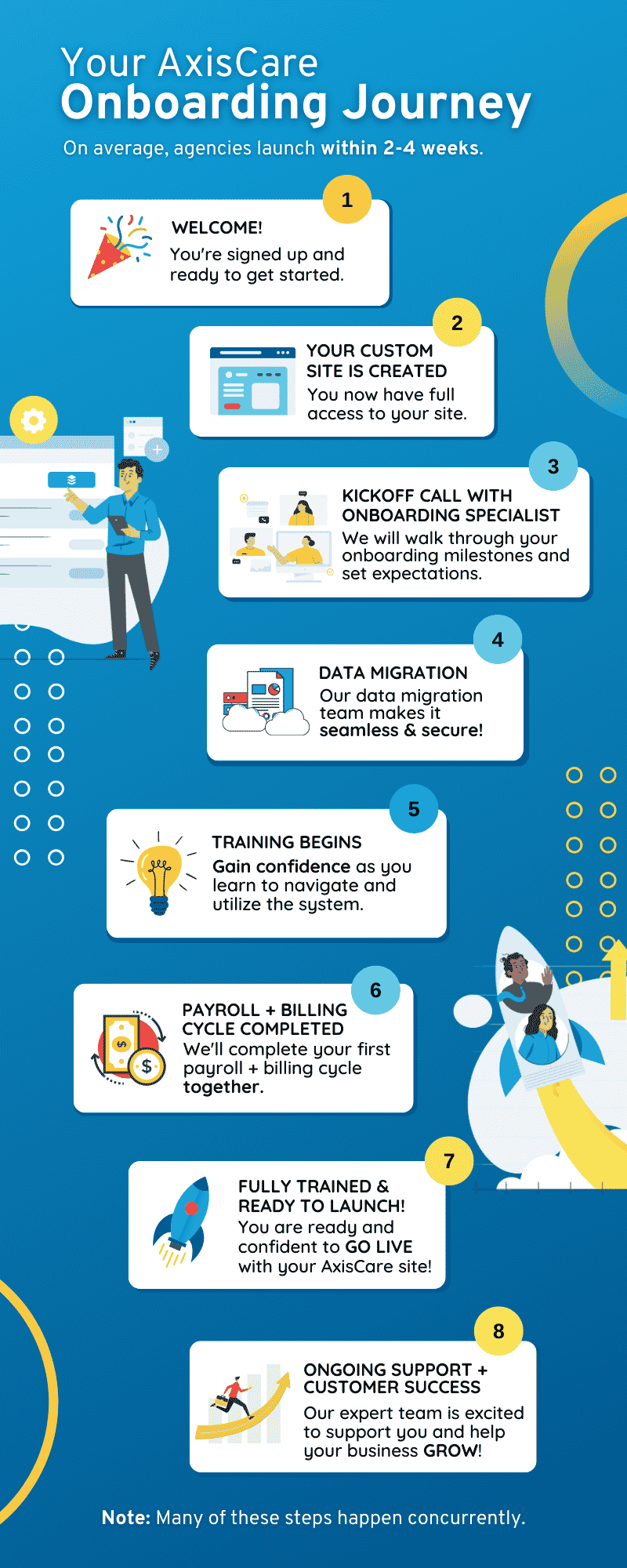
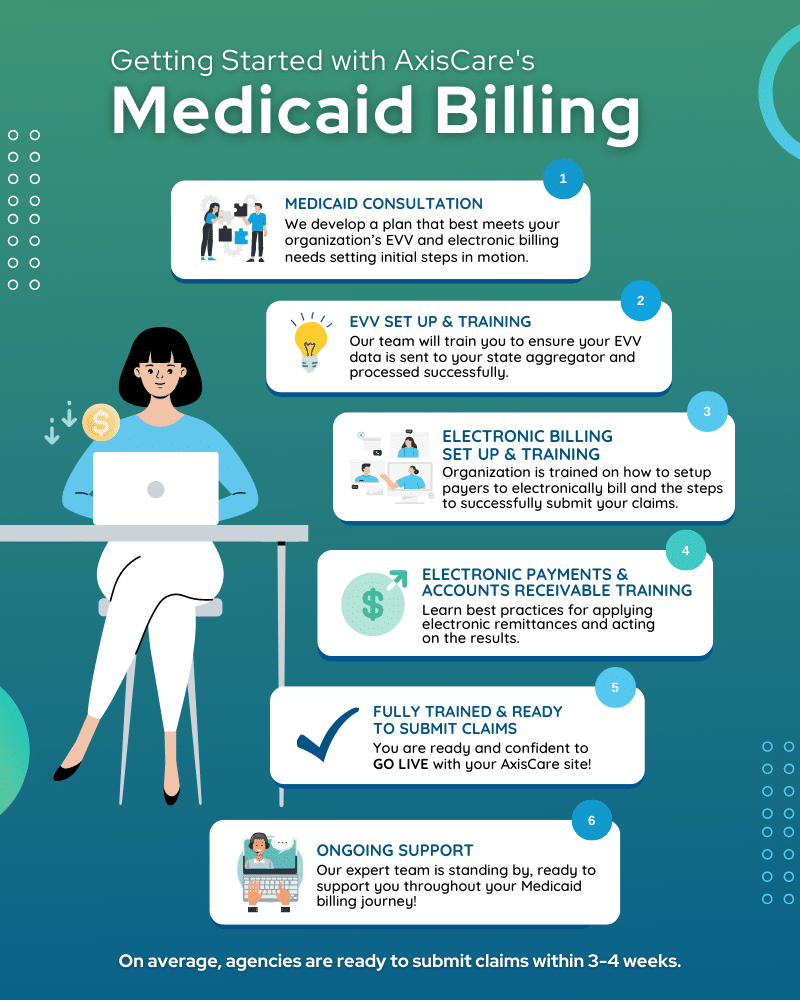
Embracing an all-in-one solution can help your organization overcome key barriers to adopting PCC. AxisCare makes it easy for families, patients, and caregivers to stay connected with innovative features that streamline and improve the patient experience.
Request a demo to learn more about what our platform can support you.