Electronic visit verification (EVV) has become the standard for gathering information during home care appointments. Across the United States, agencies are mandated to use this technology to keep standardized, transparent, and fraud-free records of every patient encounter. So, how does EVV work in home care? Let’s start with the basics and work our way up to implementation.
Summary
EVV is mandated by the 21st Century Cures Act, and states use open, closed, or hybrid vendor models, making compliance complex—especially for multi-state agencies. Choosing a vendor should balance cost and ROI with strong data security/HIPAA safeguards and seamless integration with scheduling, billing, and payroll, supported by training and responsive support. Poor vendor fit can lead to compliance gaps and claim denials, so ongoing risk management and periodic vendor evaluations are essential. AxisCare provides an all-in-one platform that unifies EVV with scheduling, billing, and reporting.
What is an EVV Vendor?
An EVV vendor is a technology provider that enables home care agencies to track visits according to EVV protocols. The data collected by these systems usually includes caregiver clock-in and clock-out timestamps, a record of services provided, and the location of the visit.
EVV was introduced as part of the 21st Century Cures Act, a federal law passed in 2016 to improve the quality and transparency of home care. One of its many mandates was for all Medicaid-funded home care services to be logged using EVV technology, with the overarching goal of preventing fraud and waste.
While EVV may be required by law, it still offers plenty of inherent benefits for agencies nationwide. Namely, a drastically reduced administrative burden that replaces manual tracking and hard-copy paperwork with standardized digital reporting.
Understanding EVV Vendor Variations Across States
Some states allow agencies to choose their EVV vendor on an individual basis, which is known as an open-model approach. Others have chosen a closed-model approach, which mandates that all agencies use the same vendor state-wide.
Some states take a hybrid approach, where a unified platform is available but providers can use an alternate solution if it meets the necessary requirements. In all three cases, the solution must meet state and federal EVV compliance standards.
Keeping up with evolving rules and requirements can be a tall order for home care providers – especially those that operate in multiple regions. Managing inter-state EVV is a complex process that opens agencies up to non-compliance risks, making their chosen vendor’s expertise all the more important. The right vendor will keep its clients up-to-date on the latest policy changes, make it easy for them to submit accurate and well-formatted data.
Essential EVV Vendor Evaluation Criteria
If your home care agency operates in an open or hybrid state, you’ll need to do some research on EVV vendors. On the docket are cost considerations, data security concerns, and, of course, ROI.
Cost & ROI Considerations
Like any system upgrade, implementing EVV comes with a few financial obligations. The most obvious upfront costs are software licensing, mobile device purchases, and staff training. Beyond that, your agency may incur some hidden costs in the form of downtime during implementation, IT support for integration with existing systems, and any maintenance or data fees.
After the initial setup, a quality EVV vendor will show you how to save lots more money in the long run by helping set up more efficient workflows, reducing billing errors, and minimizing manual administration like data entry and compliance reporting.
Data Security & Privacy Measures
Any time an organization handles client information, data security becomes a top concern. EVV vendors must process private data from every appointment, including Protected Health Information (PHI), and adhere to HIPAA regulations that ensure a great degree of privacy.
To keep things above board, your vendor should offer end-to-end encryption, require authentication to access sensitive information, and provide role-based visibility options. Many vendors also host their software on HIPAA-compliant cloud platforms with built-in redundancy, backup, and data recovery protocols.
To round out these efforts, some EVV providers undergo third-party audits – like SOC 2 Type II and HITRUST – to independently validate their system’s integrity. These audits subject the vendor’s data handling practices to various tests, confirming that they meet the industry’s highest standards.
Streamlined Integration & Implementation Best Practices
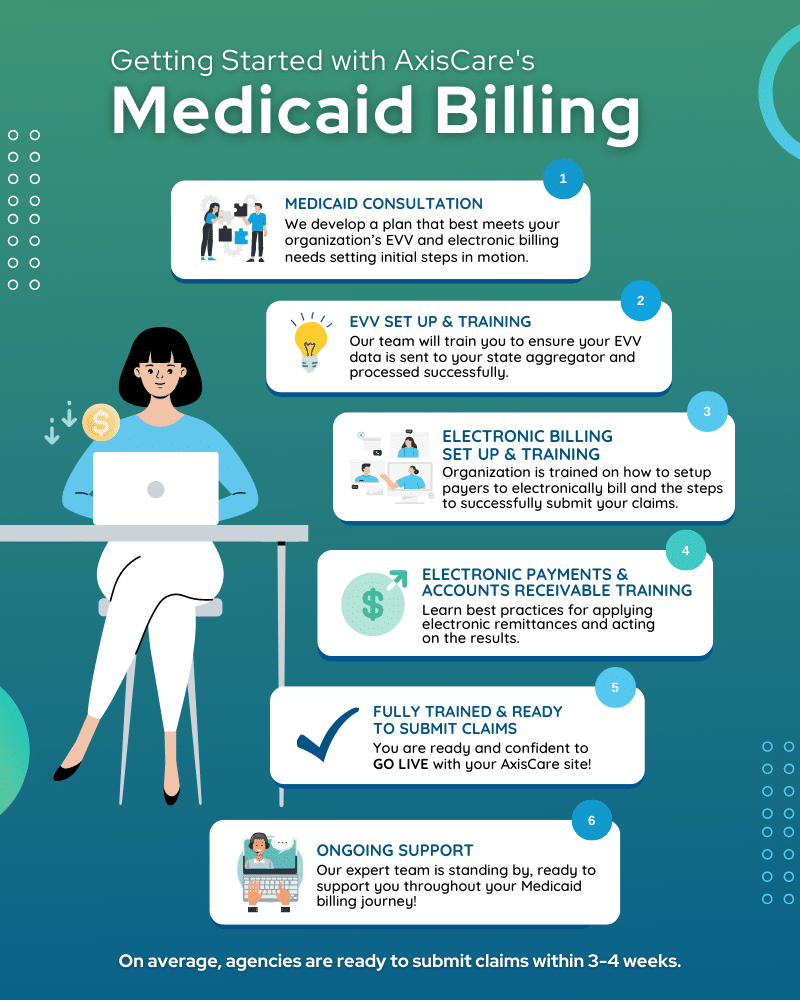
EVV is inherently tied to many other systems in an agency’s workflow. It’s connected to scheduling, as caregivers need to verify that each appointment is completed on time and in full. It’s connected to billing and payroll, as EVV data is used to verify service delivery and, in many cases, to create invoices. That’s why integrating your new solution into your existing tech stack – or, ideally, adopting an all-in-one platform – is a must.
Training & Team Adoption
Transitioning your staff to a new system will require a well-thought-out training program. The better employees understand their EVV software, the less overwhelmed they’ll feel, and the more value they’ll be able to extract. Create role-specific info sessions for different teams, provide sandbox environments for employees to experiment with features, and make post-training resources available so employees can refer back to them later.
Responsive Support Channels
Even with the most airtight training program in place, agencies shouldn’t have to walk this road alone. Transitions are challenging under the best of circumstances, and your vendor can serve as a key touch point for expert knowledge and training.
While you may not have done this before, they certainly have – so they’re perfectly positioned to handle user questions, guide staff through unfamiliar processes, and escalate complex issues quickly. Vendor support will also be in charge of making sure your software is up to date, proactively fixing bugs, improving usability, and keeping the system aligned with evolving state and federal regulations.
Addressing Common Agency Pain Points
Now, we know all about what a great vendor looks like. But what about a not-so-great vendor?
Working with a less-savvy team can spell trouble, starting with compliance confusion. EVV regulations can change on a dime, leaving agencies confused about which data they are required to log, how it should be transmitted, and what documentation is required for audits. When vendors don’t fill clients in on their updated responsibilities, agencies are exposed to compliance risks and potential payment denials.
Speaking of payment denials, billing errors are a primary source of cash flow issues. If agencies do not submit clear and accurate EVV data, even the smallest error can cause a claim to be kicked back or outright denied. Some EVV platforms don’t integrate seamlessly with billing or payroll systems, forcing admin staff to input certain data points manually. As soon as human error enters the picture, agencies are putting their financial health at risk.
Risk Management & Future EVV Preparedness
The right vendor today may not be the right one next year; your software provider shouldn’t fade out or rest on their laurels after landing you as a client. Staying on top of your EVV compliance also means periodically evaluating your level of satisfaction as a client. Internally, keeping employees up-to-date on regulatory changes will remain your responsibility – trickling that information down to your workforce is the only way to ensure your systems are working as intended.
Effectively Implement EVV With AxisCare
AxisCare is an all-in-one platform that bundles EVV tools with scheduling, billing, reporting, and so much more. Book a personalized demo with our team to find out how we can transform your operations for the better!