Tip Sheet: Medicaid Challenges That Home Care Agencies Face
For home care agencies, every payer source comes with its own set of complex rules and regulations. Ever-changing compliance requirements, lengthy repayment timelines, and pesky denials can all throw a wrench into agencies’ revenue cycles, so it’s important to stay in the know.
Understanding Medicaid’s authorization requirements, documentation standards, and more will help you avoid payment delays and general instability on the financial side of your business. Mastering these intricacies with the help of home care billing software is the most effective way to maintain profitability while consistently providing high-quality care to your clients.
The Importance of Medicaid Management for Home Care Agencies
Medicaid plays an important role in providing home healthcare access to people who would otherwise not be able to afford it. It serves as a primary payer for many clients and accounts for a significant slice of many agencies’ incomes. However, as mentioned above, it can also pose a variety of administrative challenges when it comes to billing.
Agencies have a responsibility to understand and comply with both federal and state-specific Medicaid regulations. They must keep detailed logs of every appointment to ensure they align with pre-existing authorizations, efficiently handle claim denials when they arise, and avoid cash flow issues.
Top Challenges in Medicaid Management for Home Care Agencies
For all the reasons listed above, billing management is one of the most common challenges in the home care industry. Here are some obstacles you can expect to encounter when interfacing with Medicaid.
Complexities in Medicaid Claims Processing
Billing codes categorize and identify different home care services. Caregivers log these codes during appointments, and Medicaid verifies whether the correct ones were used (or authorized to be used). Even the smallest errors can result in denied or rejected claims, sending agencies into a lengthy appeal process that requires them to resubmit the information.
Compliance With Changing Regulations
Understanding Medicaid’s complex web of regulations today doesn’t mean you’ll still be in compliance tomorrow. These rules are subject to frequent modifications, from reimbursement rate adjustments to updated documentation requirements. Not only are these policies legislated at the federal level, but each state has its own slate of rules to follow, making compliance even harder to manage for agencies operating in multiple regions.
To stay on top of the policy carousel, agencies need to invest significant time and resources into staff training and billing system updates – and even then, some details may slip through the cracks.
Coordination & Communication Issues
Avoiding miscommunications between clients, caregivers, and Medicaid administrators is a major challenge. It all starts with accurate documentation during care appointments, followed by authorization and service limit tracking on the part of administrative staff.
All of these steps need to happen quickly and precisely, as Medicaid payers require timely and accurate submissions. But if a caregiver misses a single appointment log or marks any information down incorrectly, agencies will be right back in the danger zone with payment delays and service disruptions.
Managing Data Privacy & Security
On top of Medicaid compliance, home care agencies must always stay on the right side of HIPAA. It’s a delicate dance: Medicaid asks for a lot of detailed client information that must be passed between digital systems, and the onus is on agencies to ensure it can be communicated in a way that preserves its privacy.
Striking this balance between security and efficiency can be challenging. If client data is breached or mishandled at any point, agencies become vulnerable to legal penalties, financial repercussions, and reputational damage.
Underfunding & Resource Allocation
Since Medicaid is a government-run program, its funding is at the whim of federal and state agencies. When these programs are underfunded, agencies feel the burn: reimbursement rates don’t always keep up with the rising cost of labor, administrative expenses, and service demand, forcing care providers to make difficult decisions about how they allocate their resources. They may be forced to cap caregiver wages, cut back on training, or reduce administrative support to cover their operational costs.
Methods for Overcoming Medicaid Challenges
Medicaid billing may be a beast to manage, but it’s non-negotiable for countless agencies. With the right tools in place, it’s possible to clear some of its most prominent administrative hurdles, keeping your cash flows nice and healthy.
Streamlining Claims Processing
Your administrative team is your front line, defending against rejected claims and delays. Providing sufficient training on the latest Medicaid regulations, codes, and best practices for claim submissions will substantially reduce their risk of making an error or relying on outdated information.
You can also help caregivers create complete visit logs with standardized documentation procedures, providing them with templates that guide them through all of the required information. Finally, analyze claim denial trends to identify recurring issues and adjust workflows accordingly. Over time, this will help prevent repeat billing errors and improve reimbursement rates.
Optimizing Resource Management
When resources are stretched thin, agencies must get creative with their optimization techniques. Scheduling is one aspect that is particularly prone to waste: administrators often find themselves scrambling to accommodate last-minute changes, manually matching caregivers to clients, and stuck with unassigned appointment slots.
Home care scheduling software fills these gaps automatically, pairing caregivers with clients based on granular criteria and intelligently filling unassigned shifts – no head-scratching necessary.
Ensuring Compliance & Protecting Data
In the home care industry, change is the only constant. Keeping up-to-date on regulatory changes requires a proactive attitude: agencies should subscribe to regulatory alerts like HIPAA and Medicaid-related newsletters and relevant industry publications. Joining industry associations will keep you looped in on important news in the same way. Conducting internal audits at regular intervals is also an effective way to review Medicaid billing practices, documentation, and compliance.
Strengthening Collaboration & Communication
Keeping all stakeholders on the same page about clients’ care plans and visit updates is a key part of Medicaid “hygiene.” If notes are inconsistent or garbled, that confusion might make its way into the billing process. A caregiver mobile app acts as a centralized hub for client data, acting as a single source of truth with Electronic Visit Verification (EVV) built directly into its interface.
The Role of EVV in Medicaid
EVV is a federally mandated logging system designed to maintain accurate and transparent records for Medicaid-funded home care services, requiring caregivers to digitally record details for each appointment. Its main function is to act as an accountability protocol, helping to prevent fraud, reduce billing errors, and ensure clients receive the care they’ve been authorized for.
In most cases, agencies don’t have a choice about whether or not they use EVV – it’s baked into their reporting responsibilities, whether for Medicaid or otherwise. The right technology partner will seamlessly embed this protocol into caregivers’ and administrators’ daily workflows, placing EVV-enabled apps and software at their fingertips.
Methods for Enhancing Medicaid Management
Adopting home care software marks the start of a more efficient and error-free Medicaid billing process. Here’s how automation and modern technology can help you get more claims through the door without frustrating denials.
Automated Claims Management Systems
Digital systems speed up the claims process by reducing the need for manual data entry, flagging potential issues before they snowball, and sending automated resubmissions for denied claims. Reducing friction across the entire claims process frees up precious resources, allowing agencies to refocus their efforts on client care and preserve financial stability.
Compliance & Reporting Tools
Agencies that interface with Medicaid must provide proof of compliance from time to time. Home care software has reporting tools that make it easy to generate summaries, with the ability to proactively track regulatory changes to keep your operations above board.
Data Security & Privacy Measures
Home care software has built-in HIPAA and Medicaid compliance measures thanks to advanced features like encryption. Role-based access and audit trails allow agencies to track system activity, making sure the right people are accessing the right files at the right times – no more, no less.
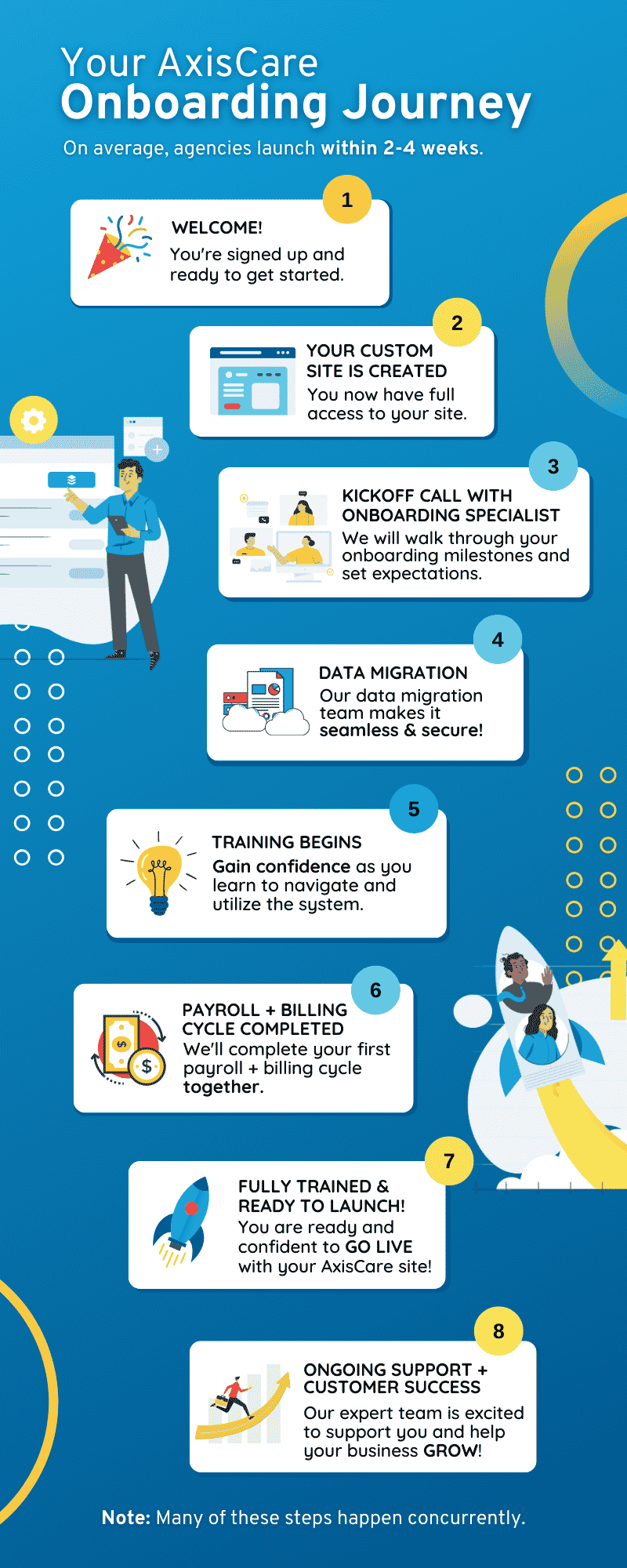
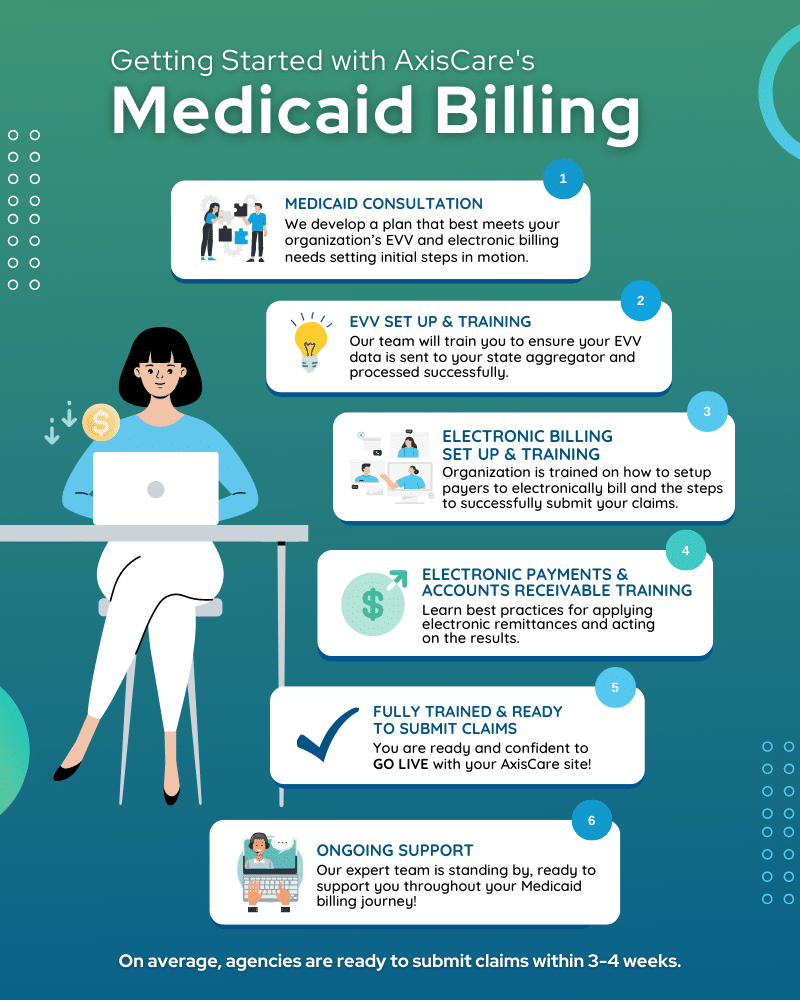
Optimize Process Using AxisCare’s Services
AxisCare Medicaid Billing takes the bulk of the work off your plate. Simply upload your referrals and authorizations to a client’s profile and our team will set up their billing information. AxisCare’s skilled professionals will submit claims on a weekly basis, handle denials and resubmissions, and update payment information in your dashboard before we send the funds directly to you.
Every step of the way, our team will help you submit clean paperwork and avoid claim denials by integrating EVV when applicable, providing customer support from Medicaid specialists, and guiding you through resubmissions when they occur.
Overcome Medicaid Challenges With AxisCare
AxisCare is designed to remove the friction from the Medicaid billing process while smoothing out every aspect of your operations agency-wide. Request a free demo to explore our process improvement solutions.