What is private pay? Every home care payer source comes with its own set of rules, and a diversified book is an important pillar of an agency’s financial health. It’s essential to understand what each source contributes to your larger revenue mosaic, how they affect access to care, how they might influence your service offering, and whether you’re equipped to deliver the right support.
What is Private Pay?
Private pay home care services are paid for directly by clients or their families. Put simply, it’s a purely out-of-pocket expense funded by one’s savings or assets – no subsidies, no outside coverage.
While insurance and government programs usually stipulate which services are within the scope of coverage, private pay offers much greater flexibility for clients; no company or governing body dictates what types of care they can or cannot receive. Payers can also seek out any caregiver or agency they please, as opposed to adhering to a list of approved care providers.
Given that this framework sees clients covering all expenses themselves, some agencies offer payment plans or financial guidance to prevent them from burning themselves out financially.
Different Types of Payer Sources in Home Care
The home care space serves a handful of common payer sources. Each one has specific eligibility criteria, coverage limitations, and application processes for clients, plus various administrative and reporting requirements for agencies.
Long-Term Care Insurance
Long-term care insurance coverage aims to ease the financial burden of home care for eligible policyholders. This type of coverage typically pays for non-medical services that support activities of daily living (ADLs), such as hygiene, dressing, and meal preparation.
To be eligible, one must demonstrate a need for assistance with at least two ADLs or have a cognitive impairment that prevents them from supporting themselves in this way. Once someone is deemed eligible, a healthcare provider will submit a claim on their behalf along with any necessary documentation.
Many policies have an elimination period of approximately 30 to 90 days before coverage kicks in, which the client must pay out of pocket. Some policies may be subject to daily or monthly benefit caps or a maximum lifetime benefit amount.
Medicaid
Medicaid is a publicly funded healthcare program that includes home care under its coverage umbrella. It covers both medical and non-medical services for qualifying individuals, though inclusions will vary from state to state. For clients with limited income and assets, it is usually the primary payer.
Given the subsidized nature of this program, individuals must meet financial and medical eligibility requirements to receive benefits. Once approved, clients will receive care from Medicaid-contracted agencies; there is limited ability to choose their own caregiver unless their specific state allows for it.
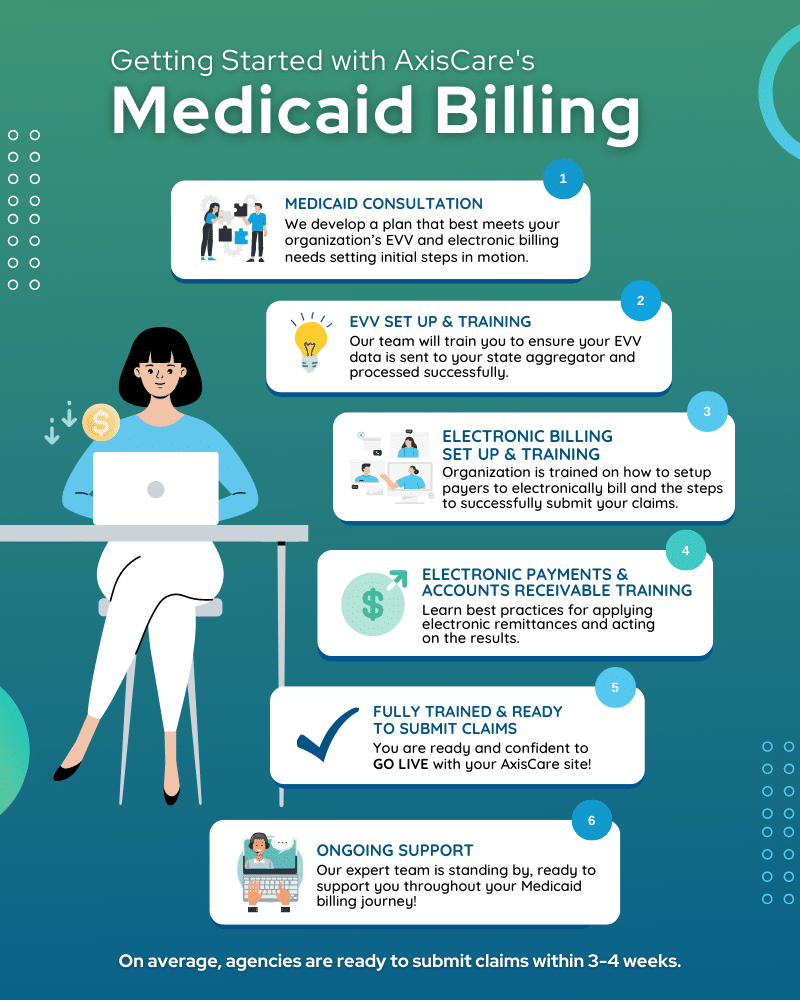
The downsides of Medicaid include long application processing times, waitlists for waiver programs, and restrictions on the number of service hours clients can claim. On the agency side, Medicaid billing can be a boondoggle, requiring strict adherence to service and reporting protocols.
Veterans Affairs (VA) Benefits
The Department of Veterans Affairs (VA) helps subsidize several home care program types for eligible veterans. In addition to providing care during active duty, the VA’s goal is to help them remain comfortable and cared for at home once their service has concluded.
One key VA program is the Homemaker and Home Health Aide Care program, which delivers personal care services through VA-contracted agencies. Home-Based Primary Care provides medical services for veterans who cannot leave their homes due to physical limitations, and the Aid and Attendance benefit offers financial support for those who need help with ADLs.
As long as potential clients are already enrolled in the VA healthcare system, the only barrier to entry is a clinical assessment. If someone is eligible, their VA physician will prescribe the necessary care and coordinate with the client’s social worker or care team if applicable.
Agencies have an opportunity to play a key role in educating veterans and their families about the care options available to them. Teaming up with VA care coordinators and offering hands-on guidance throughout the application process can support the VA’s mission of providing essential support for veterans. Internally, it’s important for agencies to brush up on their knowledge of VA billing and consider how their current service offering aligns with what’s covered by the associated government programs.
Workers’ Compensation
Workers’ compensation is a type of insurance provided by an employer. It is used to subsidize medical and non-medical care in the event of a work-related injury or illness, from assistance with ADLs to more intense interventions, especially if the client is temporarily or permanently disabled due to the incident.
Workers’ compensation kicks in when the injury or illness is reported and accepted by the employer’s insurer. Then, a physician prescribes home care to support the employee’s recovery or long-term care.
Once the new client is set up and receiving home care services, the agency must remain in close contact with the client’s case manager or insurance provider. That way, they can ensure they remain compliant with the prescribed care plan and billing requirements. As with most insurance or government-related programs, agencies must keep meticulous records of the services provided and submit progress notes to meet compliance standards.
Other State or Community Programs
Low-income seniors, individuals with disabilities, and family caregivers may also be eligible for support from state and community programs. Some offer a sliding-scale payment model, while others cover home care costs at no charge to the client.
In addition to Medicaid and federally subsidized care, these assistance programs help cover the cost of home care for specific, usually vulnerable populations. Depending on the initiative, they may help fund personal care, respite services, accessibility-related home renovations, or assistive technology.
State departments of aging, disability services, or local Area Agencies on Aging (AAAs) typically administer these programs. Since they are state-run, eligibility and benefits will vary depending on the client’s location.
Why Understanding Payer Sources Matters
Understanding different payer sources isn’t just about knowing who you need to bill. It means having a grasp of what different populations need in terms of care, who is eligible for which services, and how your agency can identify and fill gaps in the provider market.
The more agencies know about the available payer options, the better they can guide clients through the complex eligibility and application process for each one. On a more basic level, they can help guide individuals towards the best type of care for their situation, and even educate them about subsidized programs they may not know exist.
Through an operational lens, understanding different payers is the key to smoother authorizations, faster reimbursements, and fewer compliance issues. These processes and requirements tend to be very opaque, so knowledge is power when working with payers of all kinds.
Navigate Payment Sources With AxisCare
AxisCare helps home care agencies across the United States achieve operational excellence, and managing diverse payer sources is a core pillar of our work. Our software integrates with different payer systems to simplify and unify the entire workflow, from client management to invoicing and reporting. Request a free demo to see how our powerful feature suite can reduce claim denials and speed up your revenue cycle.