Understanding IDD Compliance
IDD compliance refers to the set of regulations and standards that govern the delivery of care services to individuals with intellectual and developmental disabilities. These rules are administered at both the federal and state level, meaning certain requirements will vary depending on an agency’s service area.
Broadly, IDD compliance encompasses laws such as:
- The Health Insurance Portability and Accountability Act (HIPAA) for privacy and security
- The Americans with Disabilities Act (ADA) for accessibility and non-discrimination
- Medicaid regulations that define which services qualify for reimbursement
To qualify for said subsidies, agencies must follow specific rules surrounding the appropriate authorization, documentation, and billing processes.
Why IDD Compliance Matters in Billing & Payments
In IDD services, person-centered planning ensures that supports are tailored to each individual’s needs, goals, and preferences. But even the most thoughtful plan can fall short if billing and documentation practices don’t align. Accurate, timely billing plays a critical role in maintaining uninterrupted services, as even small coding or documentation errors can lead to claim denials, which can result in a lapse in care, creating a ripple effect that affects the individual’s sense of stability.
From a financial standpoint, failure to meet the necessary requirements can significantly disrupt an agency’s cash flow. Non-compliant claims can delay payments and increase denials, leading to lengthy appeals processes and extra administrative work. Agencies may also be fined for non-compliance, suffer reputational damage, or be flagged for an in-depth audit, which demands plenty of time and resources in its own right.
Understanding and following billing requirements protects an agency’s financial health and ensures each individual will receive quality care without interruption.
Core Regulations Impacting IDD Billing
The IDD billing process is subject to many different federal and state-level regulations. From documentation requirements to data privacy, here’s what to look for.
HIPAA & Data Security
HIPAA is a widely adopted standard for handling and protecting sensitive health data. It includes provisions that apply directly to care billing, including services geared towards individuals with IDD. Meeting these standards protects the individuals’ privacy while strengthening an organization’s integrity and credibility.
Providers must use secure, HIPAA-compliant digital platforms to process invoices and submit insurance claims. All personal health data that passes through these systems must be encrypted, accessible only to authorized employees, and attached to an audit trail. Organizations keeping physical records must store them in a secure database to avoid tampering or unauthorized access.
IDD providers must comply with all of these privacy stipulations to avoid the risk of fines, penalties, and other consequences. They are also responsible for keeping their teams up-to-date on the latest data privacy requirements.
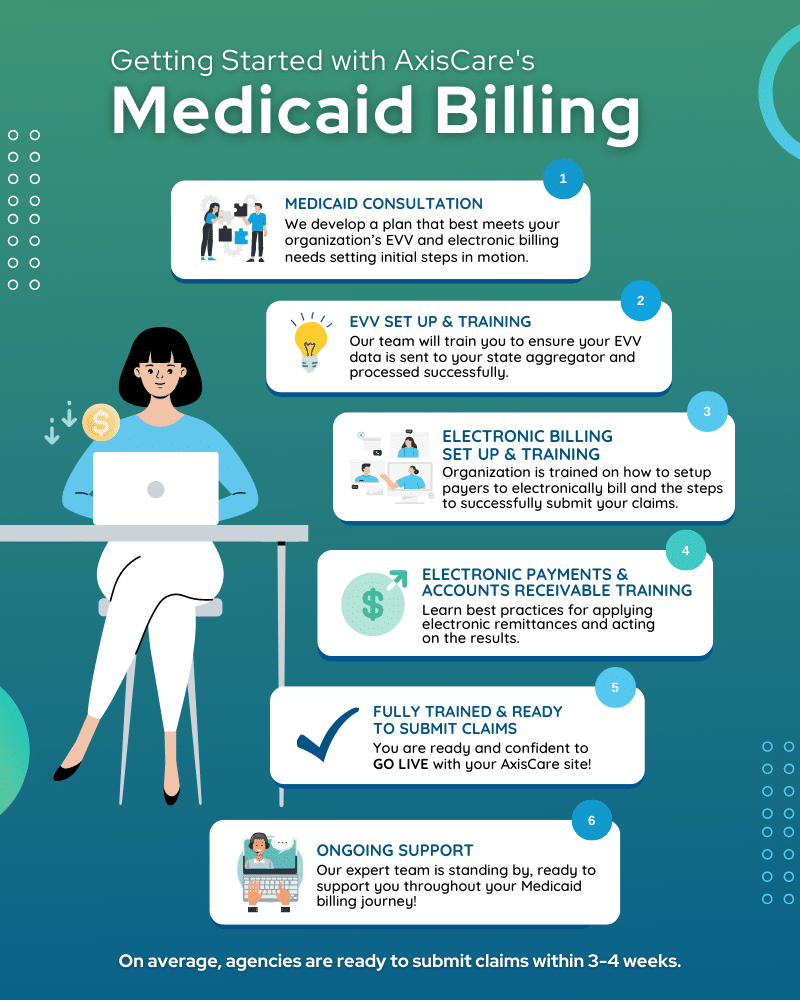
Medicaid & State-Specific Rules
Agencies also need to monitor Medicaid billing rules and evolving state-specific compliance mandates. To be eligible for Medicaid coverage, the IDD services provided must be:
- Authorized in the individual’s service plan
- Delivered by qualified staff
- Properly documented with dates, times, and progress notes
Finally, they must be billed using the correct service codes and modifiers.
Since Medicaid receives funding from both federal and state governments, billing requirements will also vary by state. Billing manuals, audit protocols, tracking protocols (like Electronic Visit Verification), and documentation standards are always subject to change, sometimes with very little notice, putting the onus on providers to keep a close watch on industry changes.
Building an Effective IDD Compliance Program
A well-rounded compliance program can turn routine tasks into trackable processes, from assessing risks and defining policies to training, internal reporting, and auditing.
Risk Assessment & Policy Development
Routine risk assessments provide a structured approach for reviewing your current workflows while looking back on past claims for errors or noncompliance. Over time, patterns will reveal themselves, offering a clearer picture of how well your organization meets the appropriate billing standards.
While data analysis can highlight many areas of improvement, going one step further and seeking input from your team, including billing staff and direct support professionals (DSPs), can help identify gaps that may not be visible in the data alone.
Agencies can compile these findings in a policies and procedures document that clearly defines expectations for billing, payment processing, documentation standards, and data security. These documents should be easily accessible to all relevant staff members and act as a single source of truth for processes like service authorization, appointment logging, and billing error correction.
It’s important for organizations to conduct risk assessments regularly, and it’s equally valuable to review and update policies as often as needed. Incorporating policy reviews into annual compliance training will keep staff informed, aligned, and accountable.
Best Practices for Accurate IDD Billing & Payments
Getting claims approved, receiving on-time payments, and remaining compliant with all relevant regulations starts here.
Verify coding and documentation
- Match the correct service codes and modifiers to each person’s service plan and state billing guidelines.
- Document services in real time to keep accurate and complete records.
- Ensure the information on billing entries and documentation is accurate to avoid claim denials and audit risks.
Always be checking
- Implement a review process to double-check claims for errors or missing information before submitting them.
- Perform random internal claim audits to catch potential issues and identify patterns of noncompliance.
Let technology do the heavy lifting
- Use electronic health record (EHR) systems to automatically log visit information and create compliant records.
- Automate coding and billing workflows wherever possible to reduce human error and streamline claim submissions.
Proactively keep tabs on compliance
- Subscribe to newsletters, updates, and webinars to stay updated on Medicaid, state-level, and payer requirements.
- Document and address billing errors promptly, including issuing corrected claims.
- Create a compliance checklist to guide employees through the billing process and reduce errors.
Prioritize IDD Compliance With AxisCare
Don’t leave your compliance up to chance. AxisCare integrates with various billing payers, including Medicaid, to ensure that every claim is accurate, compliant, and complete. Request a free demo to learn more about how we help IDD service providers deliver high-quality services while maintaining strong financial oversight.