Individuals with intellectual and developmental disabilities (IDD) require specialized support from trained health professionals. Often, these support services are provided by an IDD agency that employs direct support professionals (DSPs) who visit individuals at home or within the community. Delivering care to their doorstep is a great way to help individuals with IDD manage their unique challenges in a familiar space, which is key to preserving their autonomy and maintaining a stable environment.
At the end of each visit, direct support professionals (DSPs) must log specific data that will eventually be used for billing purposes. This information must be detailed, complete, and error-free in order to meet compliance standards and ensure timely reimbursements from payers like Medicaid and state programs. Here’s how IDD agencies are leveraging technology to keep their records spotless and their finances in check.
Understanding IDD Billing & Its Importance
IDD billing is the process of submitting and managing claims for services provided to individuals with IDD. These services may be subsidized under government plans, like Medicaid and Medicare, or reimbursed through state and private insurance programs. Each one requires a specialized billing process complete with specific codes, documentation requirements, and regulations mandated by federal- and state-level governing bodies.
Especially when interfacing with government agencies, it’s critical to submit accurate bills in a timely manner to maintain a healthy cash flow. Even a small mistake or omission can delay payments or incur penalties for noncompliance. It’s important to submit claims as soon as possible to account for processing delays that may occur within these departments.
Key Challenges in IDD Billing
A combination of elaborate government regulations and evolving Medicaid requirements makes IDD billing a heavy lift for most agencies; it’s not easy to stay current and compliant when the rules are constantly in flux. Each IDD service requires precise coding and documentation to prove its medical necessity and meet payer guidelines, and a single missed signature or incomplete progress report can trigger a denial or delay.
Relying on manual billing processes makes agencies more vulnerable to cash flow issues. It’s much more difficult to cross-reference documentation and keep it up-to-date when using paper-based systems; these inefficiencies can slow the reimbursement process and increase the administrative burden placed on staff, which ultimately pulls their focus away from client care. Over time, an accumulation of compliance violations can open agencies up to intensive audits and even reputational damage.
Best Practices for Accurate & Compliant IDD Billing
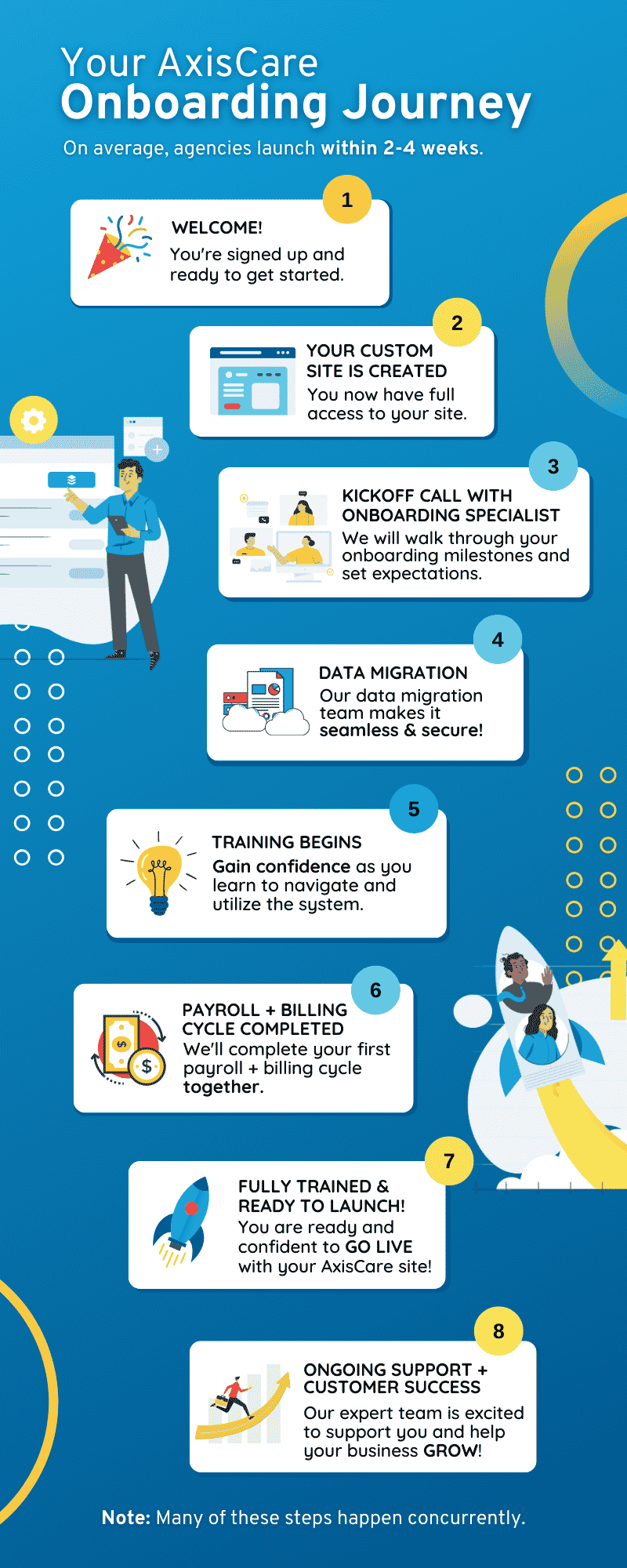
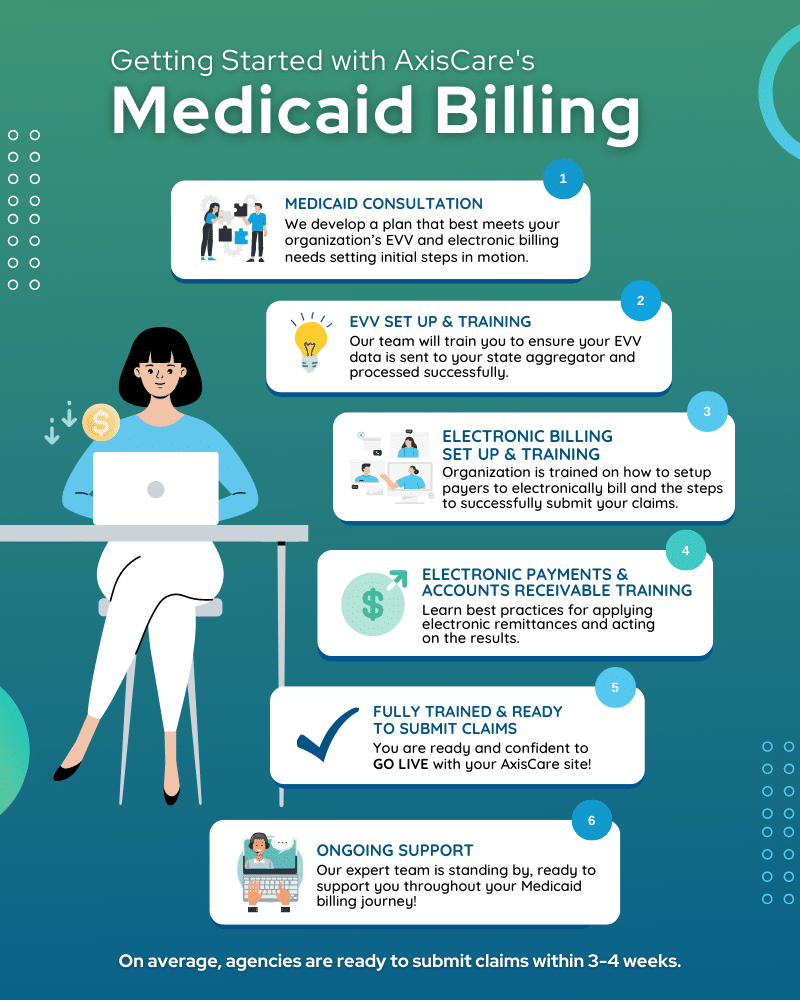
Software designed to support IDD billing and compliance is the key to avoiding costly errors and omissions. These digital tools prompt DSPs to collect a standardized set of data during each appointment, verify that service codes match the provided documentation, and automatically incorporate compliance requirements set forth by various payers.
IDD software can also automate the process of verifying billing details against service authorizations and payer guidelines. This includes confirming eligibility, approved units, and authorization periods to avoid billing for non-covered services and running into trouble.
Though technology clearly goes a long way towards reducing the risk of errors, it’s still important for employees to stay current. Regular staff training is an important piece of this puzzle, as it keeps teams informed on changing regulations, Medicaid updates, and internal billing protocols. Agencies should also conduct routine internal audits to catch potential issues early and maintain compliance.
Documentation & Audit Readiness
If your agency is well-prepared for an audit, you have nothing to fear. While the process may be laborious, everything will go much more smoothly with clear, comprehensive documentation at the ready.
To strengthen IDD billing processes with an eye toward future audits, agencies should adopt best practices that prioritize accuracy, compliance, and efficiency. Auditors often request detailed documentation to verify that billed services were authorized, delivered as described, and compliant with regulations; using the correct codes and modifiers is very important to help back up service requests and prove individuals are receiving the care that has been mandated in their plans.
Digital solutions make this process far more manageable by centralizing any documentation an auditor might require and making it easy to retrieve. IDD software allows providers to quickly access client notes, service authorizations, and billing histories, ensuring they can respond to audit requests quickly. Built-in alerts and compliance checks can also flag missing or incomplete records before they become liabilities and trigger an audit all on their own.
Maximizing Reimbursement & Cash Flow
Clean claims submissions start with clean data, and mobile apps are an easy way for DSPs to track critical information on the go. Instead of taking freeform notes, they can log appointment data in a templated standardized format within the app. They’ll be prompted to enter all of the necessary information, which in turn helps curb accidental omissions. Digital systems can even integrate with EHRs and scheduling tools to pull documented care data directly into the billing process, creating a faster and more accurate workflow than ever before.
IDD billing platforms also automate the process of claim scrubbing, flagging potential errors before submission, and providing real-time updates on the status of active claims. Staff can track payment trends via dashboards and reports, both of which help to identify bottlenecks and forecast cash flow once enough data has been compiled. Over time, chronic causes behind delayed payments and other snags will reveal themselves, pointing agencies towards the most urgent issues affecting their billing health.
Enhance IDD Billing With AxisCare
AxisCare’s advanced billing features help IDD agencies improve their accuracy, compliance, and operational efficiency. From integrations with Medicaid to robust reporting tools, our software is built to support IDD agencies’ success. Book a free live demo to learn more about how we can customize our solution to your needs.