Any home-based care agency that provides services for individuals on Medicaid is already using Electronic Visit Verification (EVV). In 2016, this system was federally mandated by the 21st Century Cures Act to verify that home health services are being delivered as needed to the intended clients. Its purpose is to help curb fraud in Medicaid claims, providing a standardized framework for appointment tracking and reporting.
Since this mandate’s inception, EVV has proven its utility far beyond regulatory compliance. It’s also a key driver of administrative efficiency and improved care coordination, giving agencies the tools to significantly reduce paperwork and streamline their documentation processes.
Strengthening Service Verification
EVV systems capture key details about each client visit using a combination of GPS and biometric technology. They track caregivers’ live locations to compare against clock-in and clock-out times, coupled with fingerprint or facial recognition to ensure that the person logging the visit is who they claim to be. This multi-layered approach works to deter fraudulent reporting, reinforce client safety, and increase transparency across the board.
When service details are verifiably correct, it also makes life easier for an agency’s billing department. Payers typically have strict rules rooted in compliance about how services are invoiced; they must match up with the client’s care plan and be submitted alongside the correct service code.
Reducing Improper Payments
The real-time, verifiable service record created by EVV pushes back against “phantom care”: invoices that reference appointments that never actually happened. Each check-in and check-out is electronically stamped with the caregiver’s authenticated identity and location, making it difficult to falsify time sheets or services. By matching billing claims to confirmed visit data, Medicaid can rest assured that they are only paying for services that were actually delivered.
The associated cost savings are proven and significant. According to the Centers for Medicare and Medicaid Services, one state projected nearly $5 million of savings in the first year of EVV use alone, mainly owed to increased investigative and post-payment review capacity and a reduction in inappropriate payments.
Enhancing Accountability for Providers
With EVV closely tracking caregivers’ actions, agencies are naturally encouraged to operate above board and in accordance with regulatory requirements. Knowing that these systems time-stamped each visit encourages prompt care delivery while supporting faster incident resolution when life doesn’t go as planned.
For example, if a caregiver is late, checks in at the wrong location, or misses a scheduled visit, the system can immediately flag the issue, allowing scheduling staff to reassign the shift or follow up with the client before care gaps occur.
Optimizing Administrative Efficiency
Anything paperwork can do, EVV can do faster and more efficiently. Instead of manually logging the time, date, location, and circumstances of every client visit, EVV takes admin work off caregivers’ plates by creating an automated snapshot. There is no need to organize or maintain hard-copy documentation.
The information captured by EVV is standardized, complete, and updated in real time. The billing team can rely on this accurate information to create invoices that won’t get kicked back due to errors or omissions, and compliance teams can easily create reports that meet key regulatory standards. In the event of an audit, EVV compliance also ensures agencies will have all the information they need in an easily accessible and broadly applicable format.
Streamlining Billing & Claims Management
The health of a home care agency’s cash flows depends heavily on its billing software. Payers are very unforgiving, and understandably so: if even a single detail is out of line—an incorrect service code, a text field skipped over by accident—a claim can be temporarily delayed or denied outright.
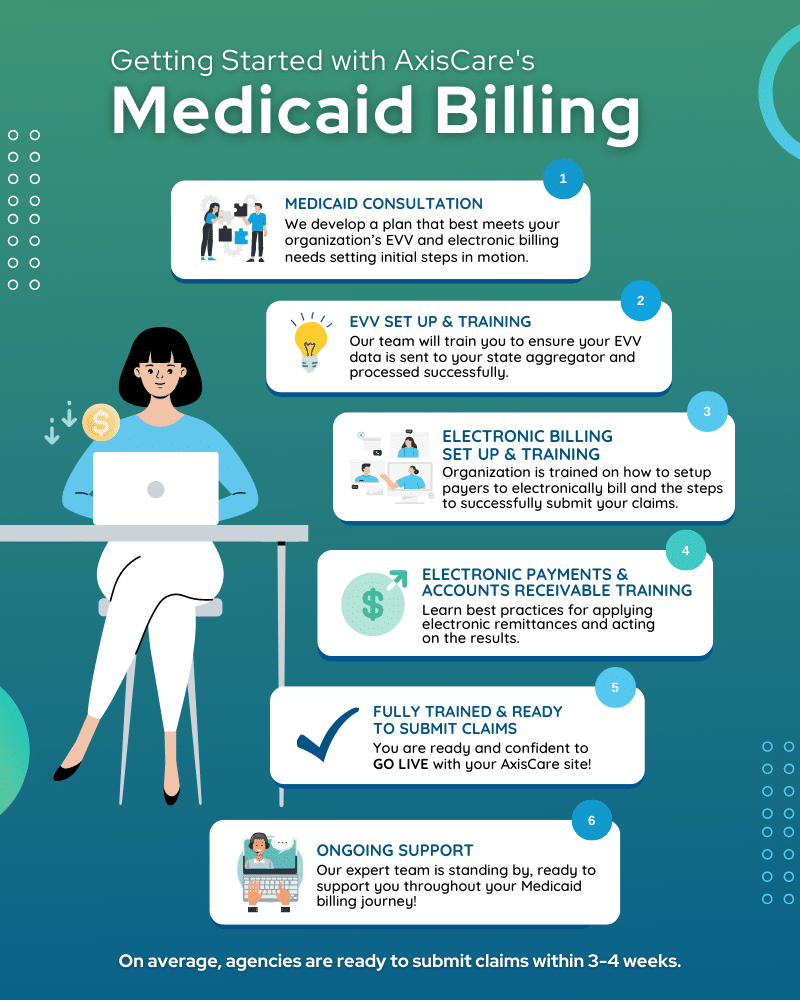
As discussed earlier, EVV’s immutable record-keeping helps eliminate mistakes or missing information; using automation, teams can send claims with greater speed and confidence. To comply with Medicaid billing requirements specifically, agencies should look for a home care platform that integrates seamlessly with their systems, from uploading authorizations to managing rejections on their behalf.
Facilitating Better Care Coordination & Outcomes
EVV paints a real-time picture of how caregivers are delivering care, enabling them to monitor punctuality, verify visit completion, and confirm that clients are receiving care that aligns with their prescribed plans. Late arrivals and missed visits are flagged as they happen, giving agencies the opportunity to quickly assign resources to open shifts and avoid service gaps before they happen.
Over time, these data points can help agencies become more proactive by identifying patterns like chronic lateness or no-shows, then deliver targeted training or staffing changes. Consistently maintaining these appointment logs also supports outcome tracking by linking comprehensive visit records to client health and satisfaction metrics.
Boosting Client Safety & Satisfaction
The most basic pillar of client satisfaction is this: did the caregiver visit happen on time, in full, and as scheduled? If the answer to this question is “yes,” agencies will be well-positioned to build strong trust-based relationships with their client base. If “no,” it’s not a lost cause just yet – but the onus is on the agency’s team to resolve late arrivals or missed appointments.
EVV alerts schedulers to these happenings quickly, allowing them to reduce the risk of care gaps that could jeopardize a client’s health while demonstrating their proactive and accountable attitude to clients and their families.
Enabling ROI & Future-Proofing Home Care Agencies
If time saved is money saved, then EVV is worth its weight in gold. By streamlining visit documentation and reducing manual data entry, this system cuts down on countless administrative hours every month, putting funds right back in agencies’ pockets. Built-in fraud prevention that leverages GPS, biometric, and phone-based verification all but eliminates fraudulent visits and other billing discrepancies, ensuring that every dollar billed is tied to a verified service. Over time, these operational efficiencies build on each other to improve cash flows and free up funds to reinvest in growth initiatives like training and technology upgrades.
If forming partnerships for the long haul is the goal, adopting technologies that establish trust from the outset is a must. Agencies that have a robust EVV system will inevitably be more attractive to payers; it acts as a “green flag” that signals accountability, built-in compliance, and smooth sailing ahead. Once they’re on board, EVV will continue facilitating a seamless claims process, positioning your agency for a strong and stable future.
Harness EVV Benefits Beyond Compliance With AxisCare
AxisCare is designed for home care agencies that want to stay on top of billing, compliance, and client management without the hassle. Thanks to our partner integrations with Medicaid and other payers, everything happens under one roof. Request a free demo to learn more.