Electronic Visit Verification (EVV) is a mandatory practice for home care agencies across the United States. As stated in the 21st Century Cures Act, organizations must use this digital system to record appointment data like services delivered, client name, and the start and end time of each visit.
Though EVV was initially implemented to combat fraudulent service records across the industry, it offers plenty of knock-on benefits for agencies. Digitizing this process helps simplify compliance, replaces hard-copy documentation, and reduces instances of “phantom care,” among other improvements. But this upside can only be unlocked if agencies smoothly integrate EVV into their workflow; if not, it risks adding to their administrative burden.
According to The Future of Home Care Trends 2026, a report sponsored by AxisCare and compiled by Leading Home Care … a Tweed Jeffries company, EVV remains a major concern for Medicaid-focused agencies. More than three-quarters of respondents agreed that ease of use, consistency, and integration with existing software systems are the most important factors for successful EVV implementation. Here’s how to make sure you stick the landing.
Common Challenges in EVV Integration
A large majority of home care agencies (86%) agree that making it easy for caregivers to clock in and out is the most important pillar of EVV software for implementation. It might not seem that important at first glance, but accurate and reliable visit reporting is the backbone of compliance and audit readiness.
If caregivers can quickly start and end an appointment using a mobile app, for example, agencies will have a reliable data set to share with regulators and the payroll team. On the other hand, a more complex process might nudge caregivers to log their hours after the fact or during a less hectic time of their day, leaving more room for error.
Integrating with existing software systems (77%) and avoiding reimbursement delays due to incomplete claims (74%) were also at the forefront of leaders’ minds. Keeping up with changing regulations (68%) rounded out the top section of this list, falling in line with the motif of lightening administrators’ workloads.
Avoiding Reimbursement Delays
Reimbursement delays throw a wrench into home care agencies’ cash flows. Waiting on Medicaid payments is a slow march as it is, and documentation errors only serve to intensify those bottlenecks. A single inaccurate data point can get claims kicked back, forcing administrators to start the process over again.
The longer it takes for agencies to get their payout, the longer they’ll need to operate with less money to go around. In the meantime, they’ll need to divert financial resources towards rewriting claims and following up instead of focusing on care coordination and caregiver support.
EVV Regulatory Importance Regulatory Importance
EVV electronically confirms that home care visits occur as scheduled and according to the recommendations laid out in the client’s care plan. It captures details like time, location, and services provided to ensure transparency and consistency in how Medicaid-funded home care services are delivered and documented.
Regulations are determined by both the federal and state governments, with different requirements set forth at both levels. The onus falls on each agency to understand the compliance requirements that apply to them, and failure to meet them can result in hefty fines. This can be an especially complex process for organizations that operate across state lines, requiring region-specific protocols under a single brand umbrella.
Steps To Integrate EVV Into Existing Home Care Systems
As you progress through your EVV integration journey, follow this roadmap to make sure you leave no stone unturned. From planning and implementing to optimizing along the way, we have you covered.
Step 1: Evaluate Current Systems & Needs
The first order of business is to determine whether you are in an open or closed model state. Open model states allow home care agencies to select whichever EVV vendor they prefer, whereas closed model states mandate that the same platform is used by all.
In rare cases, hybrid model states provide a mandated vendor, but agencies are free to choose their own as long as it meets specific requirements. If you have free rein to choose your own EVV vendor, the next step is to map your current caregiving software infrastructure to ensure your new system slots neatly into your workflow.
Step 2: Select the Right EVV Vendor
Once you’re certain that the vendor in question is certified to operate in your specific state, shift your focus over to compliance. Your platform should automatically stay updated with evolving state and federal EVV requirements, instead of placing the onus on your team to proactively seek out information (which changes frequently and often without notice).
Your EVV platform will be handling large volumes of sensitive client information, making privacy and security a top priority. Look for strong encryption features, secure data storage, and adherence to HIPAA and other relevant regulations. It’s also key to evaluate how well the EVV system exchanges data with other platforms, and whether it includes robust reporting tools that make it easy to conduct compliance audits and retrieve operational insights.
Of course, none of these features will provide much utility if your employees don’t know how to use them. Your chosen vendor should be able to accommodate the least tech-savvy members of your team: intuitive navigation and clear interfaces help minimize training time and reduce documentation errors for caregivers, schedulers, and billing staff.
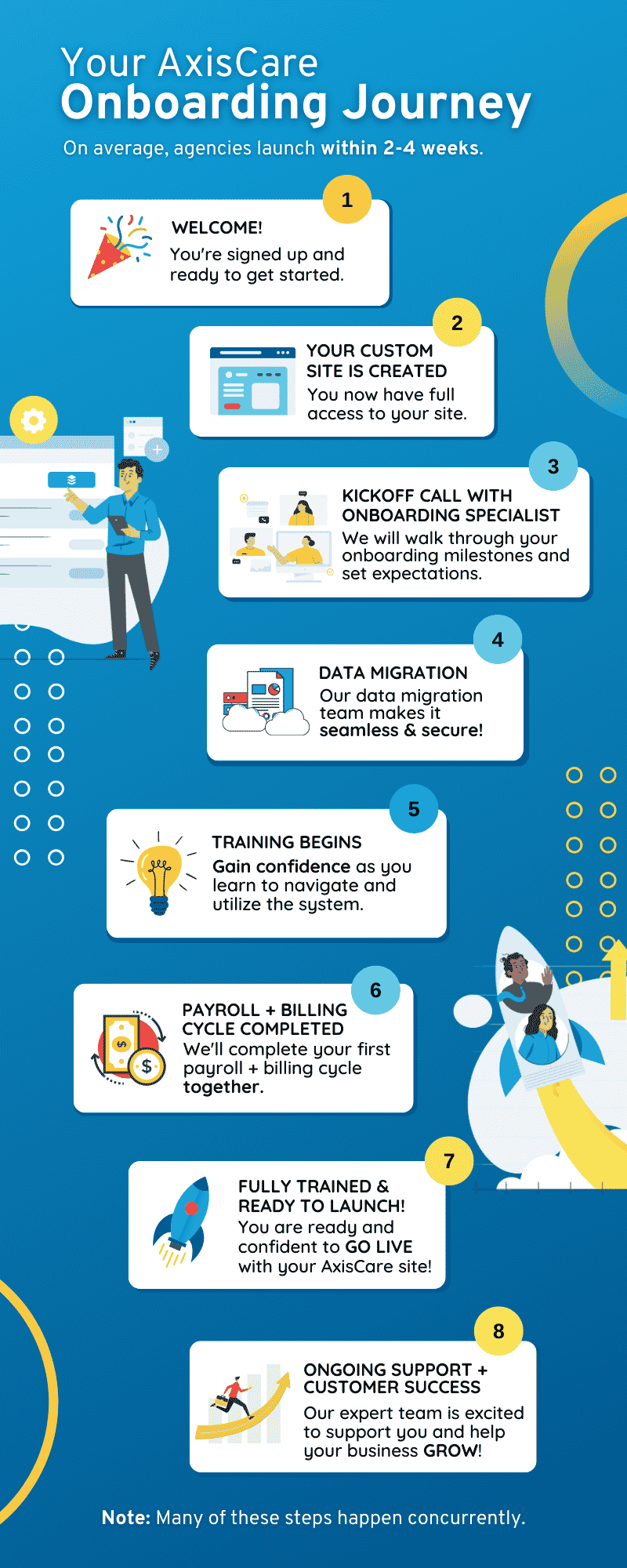
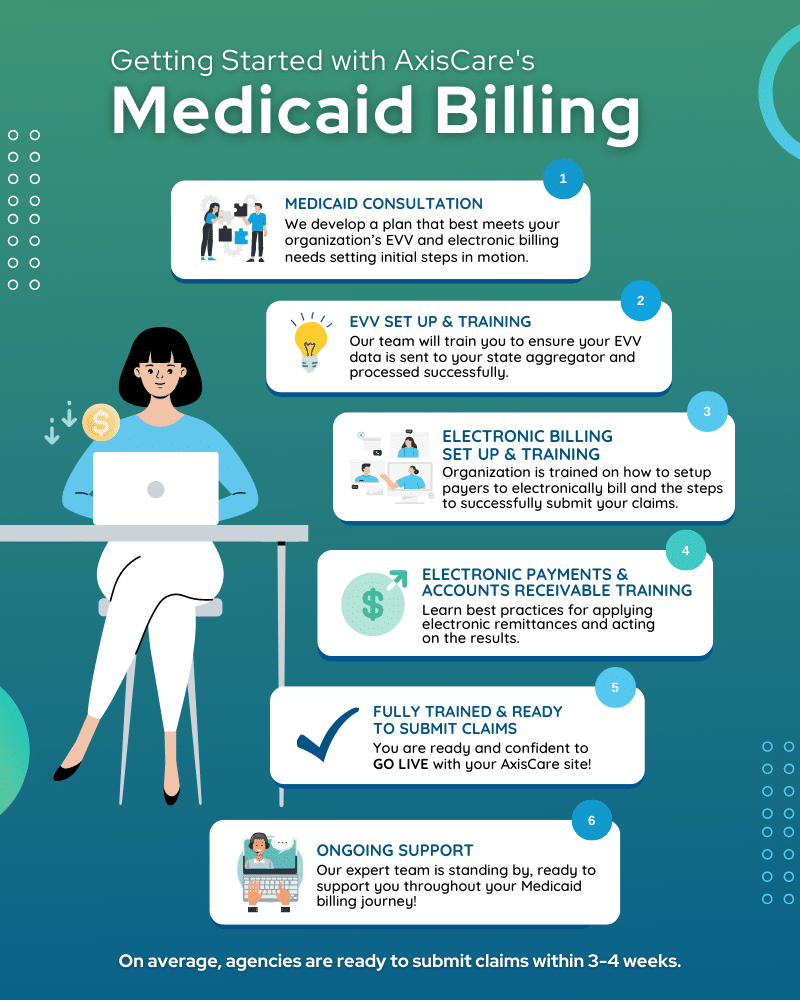
The final piece of the vendor puzzle is the quality and responsiveness of their support. A value-added vendor won’t just hand off the software and be done with you; they’ll offer hands-on onboarding assistance, training resources, and troubleshooting help to ensure smooth implementation and long-term success. The system should integrate seamlessly with existing business operations.
Step 3: Create an Integration Plan
Start defining the scope of your integration process by making note of which systems need to connect to your EVV platform (i.e. scheduling, billing, payroll, EHR) and which data elements need to flow between them. Data migration should be handled with great care, ensuring client profiles, caregiver records, authorizations, and service codes are accurate and aligned with state EVV requirements. Your IT team will be an important ally during this process, so don’t hesitate to lean on them for support!
Weave structured system testing into every phase of the process, including unit testing, end-to-end testing, and user acceptance testing. That way, you can confirm visits are being captured correctly and translating into clean, billable claims before dealing with live data.
The first phase of your rollout should entail a pilot program with a small group of caregivers and coordinators to validate real-world workflows, uncover usability issues, and refine training materials. Once those initial snags have been resolved, bring the entire organization on board.
Step 4: Train Staff & Caregivers
Successfully onboarding teams to your new EVV platform requires a thoughtful change management approach. Though many choose to implement the system in different ways, we recommend starting off by clearly explaining the “why” behind the implementation: go beyond the fact that it’s mandated by the government to explore how it protects caregivers, simplifies their responsibilities, and reduces disputes around logged hours.
Use a mix of hands-on training workshops and virtual sessions to accommodate different schedules, walking caregivers through the process of clocking in and out, editing visit information, and handling exceptions in real-world scenarios. Following the initial training, support the gradual adoption journey with easy-reference resources like short videos and step-by-step guides available on demand.
Getting supervisors and coordinators up to speed before the rest of your workforce is a good top-down approach, so they can confidently reinforce best practices and answer questions from subordinate teammates. Most importantly, establish ongoing feedback loops like check-ins and surveys to ensure caregivers feel heard and keep tabs on how the rollout is progressing.
Step 5: Monitor, Optimize, & Ensure Compliance
Compliance is a marathon, not a sprint. Agencies should regularly audit the accuracy of their data by double-checking visit exceptions, missed punches, and documentation errors. A proactive approach is the best way to catch recurring issues before they impact billing or compliance processes.
Ensuring EVV data aligns with state Medicaid requirements, including a clear trail for internal reviews or external audits, is also important for keeping the claims process running and maintaining healthy cash flows. On the technical side of things, monitoring system performance indicators like uptime and user adoption allows agencies to update their training protocols and make incremental improvements that support consistent, high-quality care delivery.
Integrate EVV Into Home Systems Successfully With AxisCare
AxisCare provides EVV support for home care agencies across the United States, helping them stay efficient and compliant in the simplest way possible. Our team is always ready to lend a hand, from the adoption phase through to post-implementation support. EVV might be mandated by the government, but we’re here to help you make the most of every feature. Request a free demo with our team to learn more.